For years, the goal of home healthcare and remote patient monitoring has been to keep patients out of the hospital for as long as possible. As RMP has grown, especially during the pandemic, people have asked, “Does RMP work with or replace home healthcare? The simple answer is, “it does both.”
They are two different services, but both have been proven to provide better health outcomes. Patients find that having healthcare from their homes is comfortable, convenient, and effective. Studies have shown a 73% reduction in hospital readmissions with these programs.
What are the differences? Home Healthcare is when a care provider is physically in the patient’s home. To bill for Home Healthcare under Medicare, your service must fit these criteria. Part-time nursing care (less than 28 hours a week), part-time home health aide, physical therapy, speech therapy, occupational therapy, and some social services.
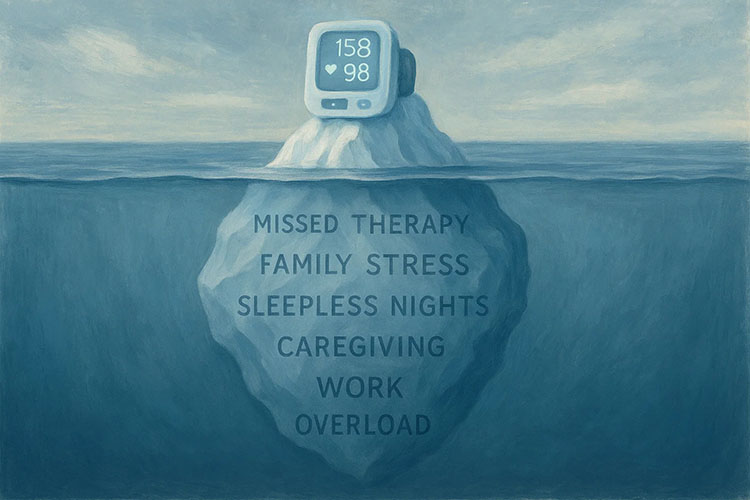
In contrast, RPM (remote patient monitoring) is a remote service that does not involve in-person visitations. Patients, with the help of smart technology, measure their vital signs from their home (or other locations). That information is transmitted in real-time, through an encrypted cloud service to a portal for a healthcare professional to review.
If a daily reading is above or below the set threshold, the RPM platform will immediately alert a clinician, who will alert the patient’s primary care physician for quick action. Doctors became aware of negative trends, spikes and anomalies immediately. RPM promotes greater patient engagement and retention. Patients can go about their day-to-day lives but also feel assured that their physician is aware of their daily health.
The billing processes is very different between these two services. With home healthcare, an agency provides the services and therefore directly bills Medicare. Therefore, the prescribing physician does not receive any financial compensation for the services of the home healthcare.
For RPM services, physicians and their staff can provide the services, or it can be outsourced to an RPM Provider. These RPM Provider companies, provide little or all of the services. Enrolling patients, sending smart devices, training patients in the devices, monitoring services, and billing services are what outsourced RPM Provider offer. As a medical practice, you can choose to use any or all of these services.
However, as the physician, you are always responsible for submitting the billing claim. Whether RPM services are insourced or outsourced, the billing physician must bill “incident to” under their general supervision.
If these are the major differences, how can RPM replace or work in conjunction with Home Healthcare? First, RPM can cost Medicare and the patients less. As a Primary Care Physician, you have more oversight with RPM than you do with Home Healthcare.
RPM cannot replace Home Healthcare in all situations. There are times when certain therapies are needed by healthcare professionals.
Yet, whichever, health plan is developed by a patient’s healthcare team, the best way to see if the plan is working is through daily health readings obtained through RPM. RPM can confirm home therapies are successful or show that a change is needed. This is how Home Healthcare and RPM work together to gain greater health outcomes.
Another reason to use RPM is the aging population. The number of U.S. adults aged 60 and older is expected to increase 30% by 2050, according to the US Census Bureau. A US News and World Report showed 88% of adults aged 50 plus, want to age in their homes. That is a large demographic who want healthcare services while they remain in their homes.
If patients can have their chronic conditions monitored in their home safely, then they are less likely to need a greater level care. RPM devices technology can provide patients with peace of mind knowing that they are being medically monitored without having to be at a facility. Coupled with in-home caregivers, the need to move patients out of their home and into more costly healthcare options is greatly reduced.
RPM Providers like Medek RPM, one of the fastest-growing companies in the US, offer a patient safety solution that can work in place of home healthcare or alongside a Home Health Agency. Both services contribute to improved clinical outcomes and help avoid potential hospitalizations.
Initiate a conversation with a Medek RPM representative to discover how RPM can assist you in caring for your chronic care patients.