Let’s start with the first CPT® Code CMS approved for RPM for direct reimbursement, CPT® 99091.
It began in 2018 when the Centers for Medicaid & Medicare Services (CMS) unbundled CPT® 99091 from other Codes. Connected Health Initiative called the establishment of CPT® 99091 “a huge victory for telehealth innovators, connected device makers, pioneering physicians, and patients across America.”
It indeed was, as it finally allowed physician practices to utilize essential connected devices to help improve the care of their patients. It would prove to be an innovation in healthcare.
While Remote Patient Monitoring (RPM) has expanded since this code was first established, it’s important to understand the basics of CPT® 99091.
So, what is CPT® 99091?
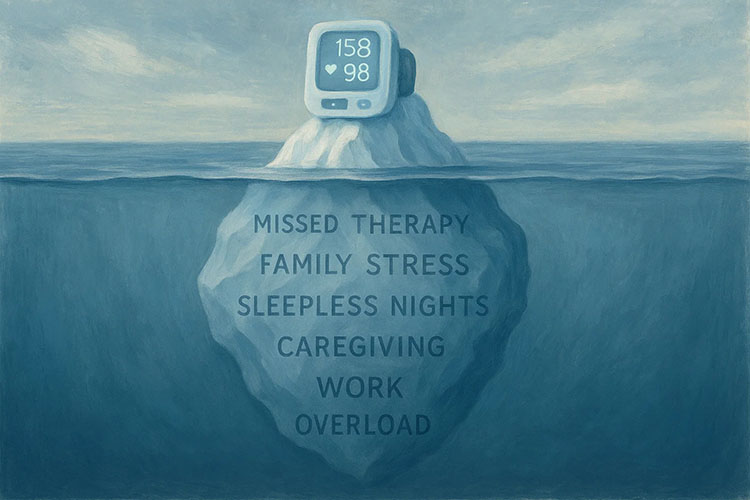
According to the American Medical Association, it is the “Collection and interpretation of physiologic data (e.g., ECG, blood pressure, glucose monitoring) digitally stored and/or transmitted by the patient and/or caregiver to the physician or other qualified healthcare professional, qualified by education, training, licensure/regulation (when applicable) requiring a minimum of 30 minutes of time, each 30 days).”
This says qualified health care professionals can bill for collecting a patient’s data using connected devices, as long as it is for cumulatively, 30 minutes a month (or more) of time spent collecting the data.
Furthermore, the American Medical Association added:
- Advance patient consent: practitioners must obtain advanced consent for the service and document it in the patient’s record.
- An in-person visit before service: For new patients or patients who have not seen a billing practitioner/provider within the past twelve months must start with an in-person visit.
- Includes evaluation/management services (levels 2-5), preventative physical exams, and transitional care management.
- Does not include virtual face-to-face visits utilizing other online or telehealth modalities.
- 30-day reporting period: billing is limited to once in a 30-day period.
This Code has since been unbundled to allow eligible practitioners to receive separate reimbursement “for time spent on collecting and interpreting health data generated by a patient remotely, digitally stored and transmitted to the provider, at a minimum of 30 minutes of time.”
Some people may find this wording confusing, which is where Medek RPM can help.
Medek RPM can make sure any practice meets all the requirements of all CMS codes. We have a team of professionals who stay on top of all the changes and work with a practice’s financial team to create the best financial return for their investment.
Our team of care professionals works with patients directly, keeping the providers up-to-date on patients’ health status and ensuring the best care.
To learn how Medek RPM can assist your practice and your patients, please reach out to us directly.