In recent years, the healthcare scene has significantly shifted, with Remote Patient Monitoring (RPM) taking the lead. But why is this? Is it just about the dramatic increase in CMS's payouts, which jumped from $5.5 million in 2019 to an astounding $53.6 million in 20221 ? Or is there more to the story?
Let's explore the top benefits of RPM and understand why it might be the next big thing your medical practice needs.
#1 Better Health Results for Patients
Remote Patient Monitoring isn't just a technological marvel; it's a lifeline. With real-time data transmission, healthcare providers gain profound insights into their patient's daily health nuances. This accessibility facilitates instant detection of anomalies, allowing for swift interventions and eliminating detrimental lag times between detection and treatment.
Furthermore, RPM paves the way for individualized healthcare. With comprehensive data ranging from vital signs to complex metrics like sleep patterns, healthcare becomes a tailored experience. This level of personalization ensures that treatments are aligned closely with each patient's needs, ushering in an era of precision medicine.2.
For patients, the result of this quick action is fewer ER visits, a significant reduction in hospitalizations, and an enhanced quality of patient care. It's healthcare optimization at its finest.
#2 Patients Get More Involved
Patient engagement is the cornerstone of successful healthcare. High-quality RPM platforms emphasize not just data collection but also patient experience. With detailed onboarding sessions, patients are equipped to navigate these systems efficiently.
Studies show that when patients actively manage their health, they feel more content and are likelier to adhere to their health routines. This is shown by an overall satisfaction boost of up to 30%3 with their healthcare provider.
RPM fosters a sense of ownership over their health journey by giving patients a lens into their health metrics. As patients continuously interact with their data, it creates an environment of proactive health management.
For healthcare providers, this elevated engagement isn't just a clinical win but a business one. An engaged patient translates to better treatment adherence, fewer missed appointments, and, ultimately, improved patient retention.
#3 Doctors and Patients Talk More
The conventional face-to-face doctor-patient interactions, while invaluable, sometimes miss the continuity that RPM brings. With RPM, annual check-ups are transformed. Instead of sporadic updates, consultations become richer, data-driven discussions, ensuring that no health detail falls through the cracks.
Beyond the annual visits, the regular touchpoints facilitated by RPM foster trust. Patients feel a constant connection with their healthcare providers, ensuring that any health issue is addressed promptly. This constancy reinforces the patient's confidence in their care.
For the engaged patient, RPM serves as an anchor. It not only ensures regular communication with their healthcare team but also ensures they have timely support. It's a holistic approach that ties together data, communication, and education.
#4 Efficiency and Time Mastery
While traditional in-office visits have their place, they are, by design, time-consuming. A national study showed doctors spend an average of 15.7 minutes with a patient4. RPM introduces an efficiency paradigm. Instead of 15-minute slots for patient reviews, healthcare providers can assess a month's worth of data in just minutes, maximizing the number of patients catered to.
This doesn't just change the dynamics for the doctors but also introduces a new operational model. With the bulk of monitoring handled either by support staff or specialized RPM provider companies, physicians can direct their attention to cases that need them the most.
In essence, RPM redefines time management in healthcare. It's about doing more with less, without compromising on the quality of care. It's about ensuring that every second spent leads to improved patient outcomes.
#5 Minimizing Risks and Liabilities
The physical act of visiting a doctor's office exposes patients to numerous potential risks, from contagious diseases to the simple wear and tear of traveling for the elderly or disabled. RPM is a beacon of safety in this regard. By facilitating at-home monitoring, it significantly reduces these associated risks.
Furthermore, for many patients, especially the elderly and those with chronic conditions, this isn't just about comfort. It's a radical shift that could mean the difference between regular healthcare management and inadvertent neglect due to the challenges of frequent hospital visits.
For healthcare providers, this model means reduced liabilities. With patients safely monitored from their homes, the chances of in-clinic transmissions or other physical risks reduce, making RPM a win-win for all.
#6 Elevated Chronic Condition Management
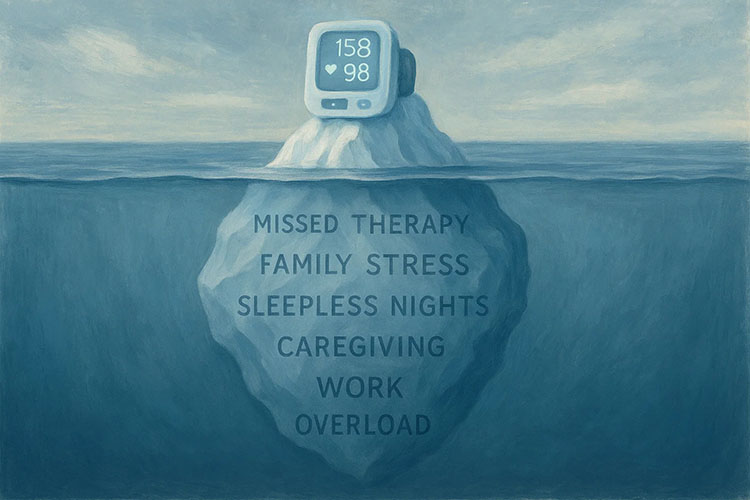
Chronic diseases require continuous monitoring and adjustment of treatment plans. RPM is perfectly aligned with this need. With the ability to constantly monitor vital parameters, adjustments to treatment can be made in real-time. This fine-tuning is especially crucial for conditions like diabetes, hypertension, and heart diseases where timely interventions can prevent major complications5.
The psychological benefits are noteworthy too. For a patient with a chronic disease, the knowledge that they are being constantly monitored acts as a comforting reassurance. It reduces anxiety and fosters a sense of security, knowing that their health is under vigilant surveillance.
For the healthcare system, better management of chronic diseases means reduced hospital admissions and a significant decrease in the associated costs. It's an approach that not only ensures better health outcomes for patients but also a more sustainable healthcare model for providers.
#7 Reducing Healthcare Costs
The financial implications of healthcare have always been a global concern. However, RPM presents a golden opportunity to significantly curb these costs. When patients are monitored regularly, it leads to early detection of health issues. This proactive approach reduces the frequency of emergency room visits and hospitalizations, thereby directly impacting healthcare expenditures.
Moreover, the decentralization of patient monitoring ensures that hospitals and clinics can manage their resources better. With fewer patients needing immediate, in-person attention, resources can be allocated to those in dire need. This optimization means less wastage and more targeted care.
From a patient's perspective, the reduced need for physical visits means fewer transportation costs and less time off work. When combined with potential savings from avoided hospitalizations or ER visits, the economic benefits of RPM become undeniable for both patients and healthcare providers.
#8 Universal Healthcare Access
Rural communities often grapple with limited access to quality healthcare. Traditional healthcare models require patients to travel significant distances for consultations, which isn't always feasible.
“..Are more likely than urban residents to die prematurely from all of the five leading causes of death,” according to the CDC6
RPM changes this narrative by bringing healthcare directly to their homes. It bridges the urban-rural divide, ensuring that geographical location is no longer a deterrent to quality care.
Moreover, these technologies can be a godsend for communities that have traditionally been underserved or marginalized. With the right infrastructure, even the remotest village can have its residents monitored, ensuring they receive timely and appropriate care.
For healthcare providers, this expansion means reaching a wider patient base. It's not just about business growth; it's about fulfilling a moral imperative — ensuring that everyone, irrespective of their location or socioeconomic status, has equal access to healthcare.
#9 Driving Research and Development
One of the less obvious but immensely significant benefits of RPM is the vast amount of data it generates. With thousands of patients being monitored, a treasure trove of health data is continuously collected. This data, when anonymized and analyzed, can offer groundbreaking insights into population health, disease patterns, and treatment efficacy.
For researchers, this is a goldmine. It provides a more comprehensive picture of real-world disease progression and treatment outcomes. Such insights can drive the development of new treatments, refinement of existing ones, and even pave the way for preventive strategies.
In a world where personalized medicine is rapidly gaining ground, the data from RPM can be instrumental in tailoring treatments to individual needs, ensuring that healthcare becomes a truly personalized experience.
#10 Reinventing Revenue Streams
In today's rapidly evolving healthcare landscape, medical practices are constantly seeking innovative ways to bolster their financial standing without compromising patient care. Remote Patient Monitoring (RPM) has emerged not only as a pivotal patient care tool but also as a significant avenue for increased revenue. CMS, recognizing the potential of RPM in reducing hospital admissions and subsequent costs, has adjusted its reimbursements to make RPM a more lucrative venture for medical institutions.
Recent challenges, including those brought about by global health crises, have prompted a shift in how healthcare is delivered and compensated. RPM stands out as a beacon in this regard. Instead of traditional office visits, which are sporadic and often limited in number, RPM provides a consistent and ongoing revenue source. A single month of patient monitoring might generate less revenue than one office visit, but its regularity ensures a steadier income flow. This is especially beneficial for practices aiming for predictable budgeting and financial planning.
Furthermore, by embracing RPM, medical practices aren't merely tapping into a temporary trend; they're investing in a future-proof healthcare model. Given the increasing emphasis on patient-centered care and the integration of technology in healthcare, RPM's role is set to expand. Medical practices that integrate RPM today are positioning themselves for sustainable growth, ensuring both improved patient outcomes and consistent financial gains.
Ready to Revolutionize Your Medical Practice?
Don't let your practice fall behind in the ever-evolving world of healthcare. Embrace Remote Patient Monitoring (RPM) today and unlock unparalleled patient care and steady revenue streams. Interested in making the leap? Connect with a Medek Representative and step confidently into the future of healthcare.
Footnotes:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10186184/
- https://www.ama-assn.org/topics/cpt-codes#:~:text=...Read%20More-,Current%20Procedural%20Terminology%20(CPT%C2%AE)%20codes%20provide%20a%20uniform%20nomenclature,claims%20processing%20and%20developing%20guid
- https://pubmed.ncbi.nlm.nih.gov/37343182/#:~:text=Survey%20results%20indicated%20that%2088.97,when%20meeting%20the%20program%20goals.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2254573/#:~:text=Average%20length%20of%20visits%20was,part%20spoke%20was%2055%20seconds.
- https://www.cdc.gov/chronicdisease/about/costs/index.htm
- https://www.cdc.gov/chronicdisease/resources/publications/factsheets/telehealth-in-rural-communities.htm